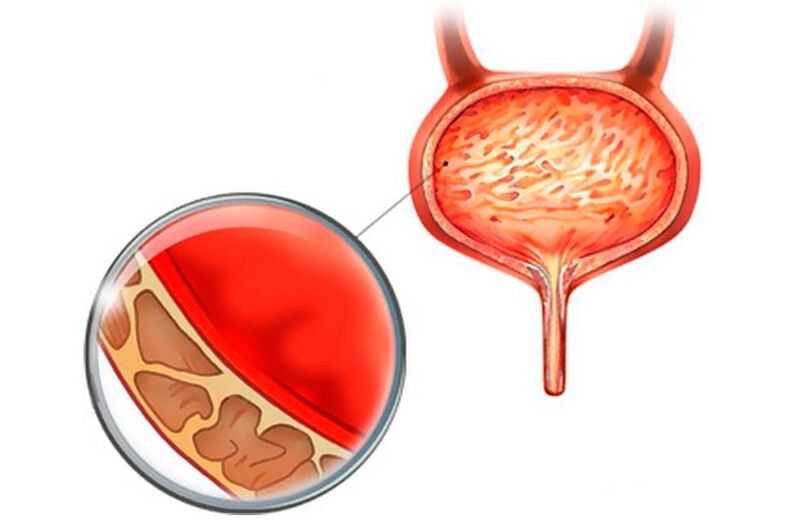
Cystitis is inflammation of the bladder wall. In practical urological terminology, the term "cystitis" is often used to denote a symptomatic urinary tract infection characterized by inflammation of the bladder mucosa, impaired function, and changes in the urinary sediment.
Signs of cystitis appear sharply:
- frequent urination (every 15-20 minutes);
- Acute pain during urination in small doses;
- blood in the urine (sometimes);
- sub fever.
If not treated right away, cystitis can become chronic, or the infection can spread up (kidney disease) or along the urethra (urethral disease).
According to statistical expertise, women between the ages of 14 and 60 suffer from cystitis at least once in their lifetime, especially sexually active women between the ages of 20 and 50 who have a history of diabetes and a weakened immune system.
As can be seen from practice, modern children often suffer from cystitis, even infants and infants. Sadly, many parents cannot predict the development of this disorder in their children.
Depending on the nature of the process, cystitis can occur:
- Acute: sudden onset with local (frequency and pain) and systemic symptoms (fever, general weakness);
- Chronic: Symptoms found on laboratory tests are slow or absent, but appear in the form of acute symptoms during exacerbations.
Depending on the causative factor, cystitis can also occur:
- Nonspecific: in the context of opportunistic pathogenic microbial communities (Enterobacter, Candida, Staphylococcus, Proteus, Klebsiella);
- Specific: Due to sexually transmitted diseases (chlamydia, Ureaplasma urealyticum, syphilis) or renal tuberculosis.
Causes of Cystitis
The majority of episodes of the disease indicate that the main cause of cystitis is infection with staphylococcus, streptococcus, Escherichia coli, as well as genital Ureaplasma infection and Mycoplasma infection, representative of the human conditional pathogenic environment.
Today, it is well known that the etiology of cystitis is clear, but it cannot be caused by just one factor.
Complicated factors that lead to cystitis:
- Sexual intercourse: The opening of the urethra is very close to the vagina and is susceptible to infection during intercourse with both female and male flora.
- Non-compliance with private hygiene rules such as daily cleaning of external genitalia, frequent changing of sanitary napkins and underwear during menstruation, cleaning of genitals after sexual contact, keeping underwear clean, and using daily sanitary napkins.
- Chronic dysbacteriosis or vaginal candidiasis: Disturbed gut and/or vaginal flora can sometimes lead to the growth of opportunistic flora, and then uncommon flora of the genital and urinary system can cause an inflammatory process that damages the entire body.
- Immune system dysfunction: Decreased immune defenses or allergic local lesions can significantly reduce the body's resistance to disease, allowing pathogens to easily enter the bladder cavity.
- Poor urination: 250-500 ml of urine can accumulate in the bladder of women, and frequent untimely emptying will lead to changes in the structure of the bladder and sphincter muscle, and create greenhouse conditions for the infection and reproduction of pathogenic microorganisms.
- The reduced protective power results in the free penetration of the infection upwards into the bladder lumen and triggers the inflammatory process therein.
- The presence of E. coli (in 70-95% of patients).
- Staphylococcus saprophyticus is present in 5-20% of patients.
- Klebsiella spp. and Proteus mirabilis (Proteus) were present in other patients.
- Bladder catheterization in men and women: Sometimes it can cause a urinary tract infection. This process is particularly dangerous for pregnant and giving birth, especially during the postoperative period when urethral tone is reduced and gram-negative bacteria show activity.
- The content of various fungi (Candida, etc. ), Chlamydia, Trichomonas, Mycoplasma and viruses in the body.
In the acute form of cystitis, a woman may become ill several times, and the disease tends to become chronic.
In men, cystitis usually occurs rarely after inflammation of the urethra, prostate, epididymis, and seminal vesicles. Among men with prostate adenomas, there is an increased likelihood of developing cystitis during bladder intubation, one of the symptoms of which is persistent urinary retention.
symptoms of cystitis
Cystitis is a very unpleasant, painful disease that can cause a lot of discomfort and pain to patients, who often endure bravely without realizing the dangers that can subsequently lead to complications from uncured cystitis. Usually, acute cystitis occurs suddenly, and postcoital cystitis occurs 8-10 hours later.
The symptoms of cystitis are very painful, the most typical of which are:
- pain when urinating;
- burning and cutting at the end of the act of urination;
- lower abdominal pain, sometimes unbearable;
- A feeling of incomplete emptying of the bladder;
- Sometimes incontinence with a strong urge to urinate (more common in children);
- cloudy or bloody urine (hematuria);
- Sometimes there is a slight increase in body temperature accompanied by a mild chill.
A rise in temperature during cystitis may also indicate possible inflammation of the kidneys or other areas, so it makes perfect sense to contact a specialist immediately.
It is known that women and girls are more likely to develop cystitis than men and boys. Curiously, the likelihood of developing cystitis increases significantly during pregnancy, although any disease is highly undesirable during this period. Many times, cystitis occurs in the early stages of pregnancy, sometimes before the woman even knows it. For everything else, cystitis is often referred to as a nonspecific or relative sign of pregnancy.
Cystitis in early pregnancy presents with the following symptoms:
- Pain that can vary from moderate pain in the lower abdomen and mild soreness at the end of urination to severe, cutting incontinence pain;
- frequent urination with small amounts of urine;
- Urine may have a pungent odor and be dark in color;
- Persistent pain in the lower back;
- slight hematuria (not always);
- fever (optional)
- Menstrual disorders in women of childbearing age.
In the elderly and children, symptoms of cystitis tend to be less pronounced. Fever, abdominal pain, and nausea may be the only symptoms of cystitis.
For diseases such as cystitis, symptoms and treatment always depend entirely on the patient's sense of responsibility for their own health.
Prevalence of cystitis
Acute cystitis is one of the most common diseases in urology. Most often, simple cystitis is observed when the bacteria affects only the bladder mucosa, while the submucosa remains intact.
According to scientific and statistical studies in the practice of urology, the prevalence of cystitis in women is 500-700 cases per 1000 patients, while in men between the ages of 21 and 50 there are only 6-8 cases per 1000 men with cystitisThe acute form is rarely observed.
The higher prevalence of cystitis in women is due to:
- Women's urethra (urethra) is shorter and has a wider lumen than men's urethra;
- The external opening of the female urethra leads directly to the perineum, which facilitates easy penetration of infection from the reproductive tract;
- The external opening of the urethra is located near the anus, which causes 80% of cystitis cases to be caused by infection with intestinal bacteria (E. coli) that enter the bladder from the intestinal lumen.
Cystitis is three to four times more common in girls than in boys. Cystitis is extremely rare in neonates and children under 1 year of age, and the disease is usually detected between 1 to 3 years of age and adolescence (13-15 years), but is most common in children 4 to 12 years old.
Cystitis in summer
Curiously, however, cystitis cases become more frequent during the warmer summer months, especially during the holidays, when most women go on vacation to other climate zones, for the following reasons:
- Vacation accommodation that does not provide high-quality hygiene care in intimate settings;
- hypothermia after prolonged bathing in a cold reservoir;
- failure of the usual way of urinating (flying, moving, new places) when you have to endure it for a long time;
- drastic changes in climate zones, resulting in decreased immune system function;
- Often increase sexual activity on vacation, etc.
If you suddenly cannot avoid cystitis while relaxing at the resort, you should contact your urologist urgently. To confirm the diagnosis, a urine test and an ultrasound scan are performed.
The latest antimicrobials and antibiotics will effectively speed up your recovery and prevent complications (acute cystitis becoming chronic). The fact is that they act only on the inflammatory process in the bladder and hardly affect other organs and systems of the body, concentrated as much as possible in the urine and the mucous membrane of the bladder disease. Toxicological effects on the body are minimal.
Particularly successful in the treatment of cystitis in summer is a drug in the group taking fosfomycin, which, like other drugs in the same series, has no phototoxicity. The drug does not contain ingredients that are photosensitizing and photoreactive, it does not increase the skin's sensitivity to the sun's UV radiation even at low intensities, so it does not cause skin redness and burns, which means it can be used without violating the beachUse under health care.
Phosphonic acid derivatives are also almost completely free of side effects and can effectively and safely treat cystitis in children and pregnant women with a single dose for uncomplicated acute cystitis. Chronic and other more severe forms of cystitis can also be successfully treated with this drug, however, remedies will be administered according to a certain regimen.
Restocking your first aid kit with broad-spectrum antibiotics just in case isn't superfluous during the long-awaited summer break.
cystitis during pregnancy
The inflammatory process in the bladder can begin at any stage of a woman's pregnancy. In any case, cystitis during pregnancy is considered complex and treatment should be carried out solely under the supervision of a resident physician.
The main causes of cystitis during pregnancy:
- hemodynamic disturbance;
- Mechanical action of the enlarged uterus on the displaced internal organs of the small pelvis;
- hormone imbalance.
All of these reasons can make it difficult to empty the bladder, leading to chronic urinary retention and infection in the bladder. At the first suspicion of cystitis, a pregnant woman should immediately contact the specialist in charge of pregnancy, who will refer her to a urologist if necessary.
Cystitis in children
Cystitis in children affects younger generations of any age, but is five to six times more common in preschool and school-age girls, and the underlying causes are:
- A girl's ovaries lack the ability to produce estrogen;
- Low barrier capacity of mucous membranes and skin;
- The short, wide urethra "opens" for pathogenic microorganisms to enter the bladder;
- Inadequate or inadequate genital hygiene care;
- A concomitant disease that causes the body's immune defenses to decline.
The combined effect of these factors helps to create favorable conditions for the proliferation of pathogenic bacteria in the urethra and bladder.
Diagnosis of cystitis
Before starting treatment, it is important to uncover all the factors that contribute to the development of cystitis. A reliable diagnosis will help develop an appropriate treatment plan and provide medical advice to avoid future recurrences of the disease and prevent cystitis from turning into a chronic form.
The following studies will help urologists make the correct diagnosis:
- ask and examine a doctor;
- obvious symptoms;
- Laboratory tests of urine and blood;
- Bacteriological studies of urine and urethral smears;
- special tests for the presence of nitrites and white blood cells in the urine;
- Bladder ultrasound;
- Determine the presence of comorbidities.
If necessary, other urological testing methods can be used.
Treatment of cystitis
How is cystitis treated? The speed and quality of the treatment of cystitis and the regeneration of the bladder mucosa always depend on the timeliness of diagnosis and the choice of treatment strategies for complex diseases.
The choice of antibiotics in the treatment of cystitis is determined by the following parameters:
- the duration of the disease;
- severity of symptoms;
- the presence of concomitant factors and pathology;
- Side effects of the drug, absorption, method, rate of excretion, etc.
The effectiveness of a drug used to treat cystitis includes its suggestive strength against one or another microorganism. It should be noted that pathogenic bacteria can mutate and become insensitive to antibiotics. Decades ago, cystitis was treated with great success by many antiseptic drugs. However, one of the main causative agents of cystitis today - Escherichia coli - has developed resistance to the effects of these drugs. In addition, the previous generation of antibiotics had very high toxicity and many side effects.
The cost of treatment must also be considered when selecting a drug against the pathogen of cystitis, which is mainly reflected in the cost of the drug itself, rather than its effectiveness, long-term use, and existing risks to patients. patient's health.
Modern drugs to treat cystitis selectively act on the pathogen, concentrating in the bladder, increasing its effectiveness. The use of the latest generation of antibiotics reduces the duration of treatment for cystitis and reduces the risk of side effects, thereby reducing harm to patient health. The broad-spectrum antibiotics of the fosfomycin group are an effective and safe drug for the treatment of cystitis in pregnant women and children.
How is cystitis treated? In addition to antibiotic treatment, one should not forget about other treatments:
- Anti-inflammatory and analgesic treatment with antispasmodics;
- Stimulate and regulate the immune system;
- a diet that does not eat greasy and spicy food;
- increase the drinking regime;
- Fear of hypothermia;
- A heating pad to warm the lower abdomen;
- Eliminate anxiety and stress;
- an active lifestyle;
- phytotherapy;
- Use iontophoresis, ultra-high frequency or induction thermotherapy.
Remember that the presence of certain gynecological conditions prohibits the use of physical therapy and hyperthermia procedures.
Helpful Tips for Preventing Cystitis
To prevent and prevent the occurrence of cystitis and its recurrence, follow simple advice:
- Follow the rules of personal hygiene: wash your face at least once a day, preferably 2 or more times with baby soap (without harmful additives) and running water.
- Monitor your sexual partners for simple genital hygiene.
- Be sure to wash yourself with soap before and after each sexual encounter, and your sexual partner must do the same.
- When there are oral infections such as stomatitis, tonsillitis, and candidiasis, oral sex should be excluded to avoid infection of the external genitalia and urethra through saliva.
- Dress according to the weather, not fashion. In cold weather, the miniskirt's payoff may be cystitis, not just cystitis, but chronic, recurrent, or even adnexal inflammation that threatens years of medical procedures, infertility, and hopes of recovery.
- Note that frequent acute respiratory infections and acute respiratory viral infections indicate a weakened immune system, and steps should be taken to improve its condition.
- Try not to hold back when you want to urinate, or holding back can lead to a bladder infection.
- Stick to normal drinking patterns - 2 liters of water a day, and in high heat - drink 1-1. 5 liters more.
- Women are advised to use sanitary pads rather than tampons, as tampons can compress the urethra and become a source of infection, which can lead to bladder infections.
- It is recommended that men change their underwear every day to avoid the occurrence of non-specific urethritis as much as possible.
- When using the toilet, it is recommended to wipe from front to back rather than front to back to avoid introducing gut bacteria into the external genitalia, from there into the urethra and bladder.
Following these tips will not eliminate 100% cystitis, but it will help minimize the risk of developing the disease.





























